COVID test-and-treat: Testing and treatment (such as Paxlovid) are still free in California regardless of insurance or immigration status after the end of the public health emergency. Contact your provider or a free test-and-treat center to get treatment.
UCSF has a COVID treatment study for those at lower risk who would not otherwise be treated. Participants need to enroll withing three days of symptom onset and transportation is available. Click here for more study info.
Free COVID clinical consults for CA clinicians: California health care providers can call (866) 268-4322 (COVID-CA) to receive free and confidential consultation on COVID-19 testing and treatment from the UCSF National Clinician Consultation Center.
What to do after testing positive for COVID
- Stay home (“isolate”), wear a mask to protect people around you, and ventilate your space, including at home. Ventilate by opening windows and doors to outside air, turn on fans to face outside, turn on exhaust fans, use humidifiers and HEPA air filters if you have them. If possible, stay in a separate space from household members who don’t have infection, especially if they are at high risk, and wear a tight-fitting mask until you test negative. See CA isolation guidelines below. Roots has a helpful video on how to prevent the spread of COVID within your household.
- Contact your medical provider or a test-to-treat provider ASAP because you may be able to get antiviral treatment, even if you are vaccinated. Treatments are more effective taken as soon as possible after the start of symptoms. If you don’t have insurance or can’t reach your provider, here are some free treatment options:
- California free virtual COVID-19 visits and treatment access: phone line 833-686-5051 and website through Sesame Care. Appointments are available 24/7.
- In Alameda County, you can call the COVID-19 Community Support Team: 510-268-2101, Monday-Friday, 8:30 a.m. – 5 p.m for additional help.
- Contra Costa County residents can call 1-877-661-6230 if you test positive to reach a nurse and get a free same-day telehealth consult and prescription if medically appropriate.
- Symptom management – what you can do to take care of yourself:
- Rest and drink fluids regularly.
- Use a thermometer to check your temperature. If it’s over 100.4°F, you can take acetaminophen (Tylenol) or ibuprofen (Advil, Motrin). Tell your medical provider if you have a fever that won’t come down with these medicines.
- Use a pulse oximeter to measure the oxygen level in your blood. You can purchase one for around $20 online or at many pharmacies. If your reading stays below 94%, you should tell your medical provider.
- If needed, use other over-the-counter cold and flu medications for a runny nose, fever, headache, sore throat, muscle aches and cough (common COVID symptoms).
- If you have shortness of breath, you may get some relief from resting on your belly (prone position) rather than on your back (supine position).
- Here’s a guide for movement and exercises while recovering from COVID-19: Bouncing Back from COVID-19: Your Guide to Restoring Movement from Johns Hopkins Medicine (PDF): English | Spanish | Hindi
- Increase walking and other forms of activity as you can tolerate.
- Remember that it can take different amounts of time for each person’s symptoms to resolve and make a complete recovery.
- Keep in mind that in a small percentage of people with COVID-19, viral rebound may occur: you feel better and your antigen test becomes negative, then a few days later, the symptoms come back, and your antigen test becomes positive again. If that happens, start isolating again because you are likely infectious and let your medical provider know, as you may benefit from re/treatment.
- Get vaccinated and/or boosted if you’re due for any doses to protect yourself against reinfection and future variants. You can get a vaccine dose as soon as you’re done with your isolation period.
More detailed guidance for people living with HIV can be downloaded here: GTZ-SF’s COVID FAQs after testing positive.
California isolation guidelines
California isolation and quarantine guidelines were updated on March 13, 2023:
- If you test positive for Covid, isolate for at least 5 days and wear a mask for 10 days.
- You may leave isolation after 5 days if symptoms are gone or improving and have had no fevers for 24 hours without the use of fever-reducing medications.
- Wear a mask around others for 10 full days after start of symptoms. If you had no symptoms, wear a mask for 10 full days after your positive test. You may remove your mask sooner than Day 10 if you have two negative tests in a row, at least one day apart.
- Click here to download the Alameda County isolation PDF. Click here to read more isolation details from Alameda County.
- If you were exposed to Covid and have no symptoms, test immediately and 3-5 days after your last exposure. Wear a mask for 10 days, even at home around others.
The CDC updated unified guidance for respiratory viruses in March 2024, including guidance for Covid, flu and RSV:
- Most guidance around prevention (vaccines, hygiene, ventilation, masks) is not changed.
- Isolation guidance now is similar to California’s and includes staying at home when you’re sick, then using masks and tests for 5 days after your symptoms get better to help prevent transmission.
- Updated 2024 data on this winter season’s Covid, flu and RSV severity and vaccine efficacy is published on Background for CDC’s Updated Respiratory Virus Guidance.
These strategies will help you reduce spread to other people, as found in the study summarized in this graphic:
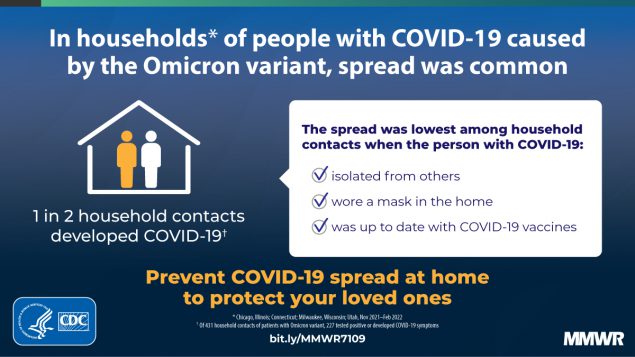
A CDC study found that household transmission for Omicron was 53%. Secondary attack rates were lower for people who were boosted (43%), people had their primary vaccine series (44%), compared to people who were unvaccinated (64%). People with infection who wore masks had lower transmission rates (40%) compared to those who didn’t wear masks (69%). Those who isolated also had lower transmission rates (41%) compared to those who didn’t isolate (68%).
Treatment options for non-hospitalized adults with mild to moderate COVID-19
Free COVID clinical consults for CA clinicians: California health care providers can now call (866) 268-4322 (COVID-CA) to receive free and confidential consultation on COVID-19 testing and treatment from the UCSF National Clinician Consultation Center.
If you’re a community member with COVID-19 symptoms, contact your health provider or a test-to-treat provider as soon as possible to see if you can get treatment. A positive home antigen test result is sufficient for diagnosis of COVID-19 (take a photo of the result if you can). The sooner you start treatment for COVID-19, the more effective it is.
Free test-and-treat options for people without insurance or a provider:
- California free virtual COVID-19 visits and treatment access: phone line 833-686-5051 and website through Sesame Care. Appointments are available 24/7.
- Click here for the national test-to-treat directory.
Below is detailed information about current treatment options and ways to access them in the East Bay. This section is very “medical” and mostly a resource for health care providers. For the latest updates, check the NIH COVID Treatment Guidelines, DHHS COVID treatment guides, and download the DHHS COVID treatment algorithm decision aid (PDF). The following was adapted for the East Bay using info from Table B in the national guidelines.
| Drug name in order of preference | Time From Symptom Onset | Dosing Regimen | Efficacy, notes and East Bay access (added) |
| Paxlovid: Ritonavir-Boosted Nirmatrelvir Oral antiviral: protease inhibitor with boosting For ages 12+ and 40+ kg | ≤5 days | • eGFR ≥60 mL/min: Nirmatrelvir 300 mg with ritonavir 100 mg PO BID x 5 days • eGFR ≥30 to <60 mL/min: Nirmatrelvir 150 mg with ritonavir 100 mg PO BID x 5 days • Not recommended for eGFR <30 mL/min or severe hepatic impairment | • 88% reduction in hospitalization or death vs. placebo and 89% reduction for unvaccinated high-risk patients in pre-Omicron studies. Paxlovid was also found to reduce the risk of long COVID by 26% in a large VA study. • Check drug interactions! www.covid19-druginteractions.org and make sure the patient’s medications EHR list is accurate. • La Clínica, hospitals and CVS, Walgreens, Safeway, and Rite Aid pharmacies have supply. Call to ensure it’s stock and send the Rx through Epic. • Check the National test-and-treat directory, the National COVID tx locator, pharmacy list and Alameda County for more sites. • Paxlovid expiration dates have been extended to 24 months by the FDA. Check updated expiration dates here. |
| Remdesivir IV antiviral: polymerase inhibitor For all ages | ≤7 days | • 200 mg IV on Day 1, followed by 100 mg IV once daily on Days 2 and 3 • Not recommended for eGFR <30 mL/min or severe hepatic impairment | • 87% reduction in hospitalization or death vs. placebo in pre-Omicron studies. • In Alameda County: check for access at Highland Hospital, Sutter Hospitals, UCSF (UCSF pts), Stanford (Stanford/Santa Clara County pts), or the National COVID tx locator. |
| Molnupiravir Alternative oral antiviral: polymerase mutagenesis For ages 18+ | ≤5 days | 800 mg PO BID x 5 days Not for use if pregnant or breastfeeding due to fetal mutagenic risk. | • 30% reduction in hospitalization or death vs. placebo; better results in a study in India, but all were pre-Omicron studies. • La Clínica, hospitals and CVS, Walgreens, Safeway, and Rite Aid pharmacies have ample supply. • Check the National test-and-treat directory, the National COVID tx locator, pharmacy list and Alameda County for more sites. |
As of December 2022, bebtelovimab was no longer recommended for Covid treatment because of BQ.1/BQ.1.1 resistance, and the FDA has withdrawn its authorization.
Promising treatment options
- Metformin (a safe and inexpensive medication usually used for diabetes) taken for 2 weeks during acute COVID infection was found to reduce healthcare utilization for severe COVID and the development of long COVID symptoms by 42% in a randomized control trial.
- Ensitrelvir (a protease inhibitor like Paxlovid) taken once a day for 5 days was compared to placebo in a randomized control trial in people at lower risk (mostly ages 12-69, vaccinated, no medical risk factors for severe disease), and was found to reduce long Covid symptoms by 26-45%, shorten symptoms by a day and reduce time to first negative test. Ensitrelvir is already approved for COVID treatment in Japan.
Viral rebound
Viral rebound is common for both treated and untreated people with COVID-19. Treatment still helps reduce disease severity, and there are no signs so far of resistance. Just make sure to re-isolate when it happens. The CDC issued a health alert on viral rebound after Paxlovid treatment and continues to recommend Paxlovid for the treatment of mild to moderate COVID-19. More data is emerging on rebounds in both treated and untreated people.
Clinical guidance on viral rebounds:
- Please counsel clients to monitor for symptoms and positive antigen tests 2-8 days after “initial recovery” (after a treatment course is completed, symptoms resolve, antigen tests become negative).
- When rebound occurs, advise people to follow CDC’s guidance on isolation, re-isolate for at least 5 days and wear masks to prevent further transmission.
- Most rebound cases reported so far have mostly been mild, with a median of 3 days of symptoms, without any evidence of reinfection or viral resistance to Paxlovid.
- The CDC says to “Consider clinical evaluation of patients who have COVID-19 rebound and symptoms that persist or worsen.” There may be cases of moderate or worsening symptoms in people at highest risk and risk for long COVID in which re-treatment may be considered with a provider. Please consider the unique situation for each patient.
- Please report cases of COVID-19 rebound after Paxlovid treatment to Pfizer using the Pfizer Safety Reporting tool. Health care providers are also encouraged to submit the FDA MedWatch form.
Data on viral rebounds:
- In one pre-omicron study, the rebound rate was 12% among untreated people.
- Anecdotal reports from East Bay clinics estimate 10-20% people during the Omicron era have rebound, and it’s higher among those who are treated with Paxlovid.
- A BA.2 and BA.5 rebound study found no resistance mutations and a robust immunologic response. Most people do not have severe disease or high viral loads during the rebound.
COVID PrEP (Pre-exposure prophylaxis)
Evusheld for COVID prevention is no longer authorized as of January 26, 2023 due to XBB and BQ resistance. The Evusheld monoclonal antibodies are no longer effective against >90% of the circulating variants, so its authorization was revoked by the FDA.
As of January 2023, there is no effective COVID PrEP available. People with immunocompromising conditions are strongly recommended to get vaccinated if they don’t have contraindications and to seek treatment immediately if they become infected with COVID-19.
Long COVID resources
Prevention of long COVID
- Protecting yourself against COVID infection and reinfection is the best way to reduce the risk of long COVID. This includes wearing well-fitted masks, ventilating, avoiding crowds, testing before gatherings, asking people to stay home when sick and staying up to date with vaccines.
- Vaccination with 3 doses reduce risk by 73%, while 1-2 doses were associated with a 43% reduction in a metanalysis and systematic review of 41 studies (mRNA vax better). For kids, a large cohort study found that VE was 24% for kids 5-11 (lower dose vax) and 50% for adolescents (adult dose vax). VE was 61% at 6m post-vax but decreased to 11% at 18 months.
- Paxlovid treatment reduced risk by 26% in a large observational VA study but did not reduce risk in another observational UCSF study.
- Metformin x2 weeks during acute COVID infection reduced severe COVID and long COVID symptoms by 42% (higher significance for female, BMI>30, unvax) in an RCT.
- Ensitrelvir (a protease inhibitor like Paxlovid) taken once a day for 5 days was compared to placebo in a randomized control trial in people at lower risk (mostly ages 12-69, vaccinated, no medical risk factors for severe disease), and was found to reduce long Covid symptoms by 26-45%, shorten symptoms by a day and reduce time to first negative test. Ensitrelvir is already approved for COVID treatment in Japan.
- A “healthy lifestyle” (BMI 18-25, never smoking, exercise, moderate alcohol intake, high quality diet, sleeping 7-9 hours per day) was found in the Nurses’ Health Study II cohort (all women, 97% white) to be associated with a lower risk of long COVID. Participants with 5-6 healthy lifestyle factors had 49% lower risk of long COVID.
Treatment and rehabilitation
- Find a Long COVID specialty center in the US; the closest ones to the East Bay are at UCSF, UC Davis and Stanford.
- Recovery guide: Bouncing Back from COVID-19: Your Guide to Restoring Movement from Johns Hopkins Medicine (PDF): English | Spanish | Hindi
- CDC’s Long COVID guidance (aka PASC: Post-acute sequelae of COVID)
- Support and advocacy groups: Body Politic, Patient-Led Research Collaborative
Long COVID studies
- Bay Area UCSF LIINC study
- National RECOVER study with sites across the US including UCSF
- National HIV Covid Recovery Study that can be done from home
Long COVID policies and advocacy
- US White House’s memorandum on Long COVID (April 5, 2022)
- Advocacy groups: Body Politic, Patient-Led Research Collaborative
