This page includes links to East Bay COVID viral levels, testing, vaccine, masking, prevention, treatment and other resources. In December 2023, we transitioned from monthly updates to posting practice-changing updates as needed. Please click here to share feedback.
East Bay COVID resources
There are still free COVID vaccines, tests and treatment in the East Bay, available to everyone in California regardless of immigration and insurance status.
Find the latest East Bay COVID wastewater viral levels on the WastewaterSCAN dashboard. You can also find COVID wastewater levels on the California state Cal SuWers dashboard and the CDC dashboard, but there are 1-2 week delays in data reporting compared to WastewaterSCAN. Click here for Wastewater FAQs and 💩 Feces Facts.
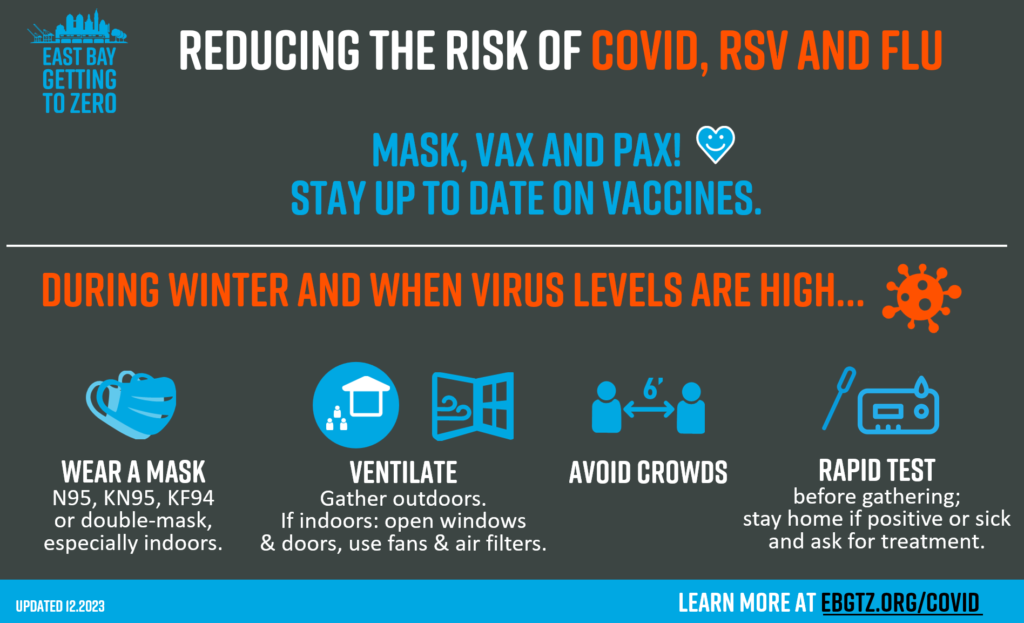
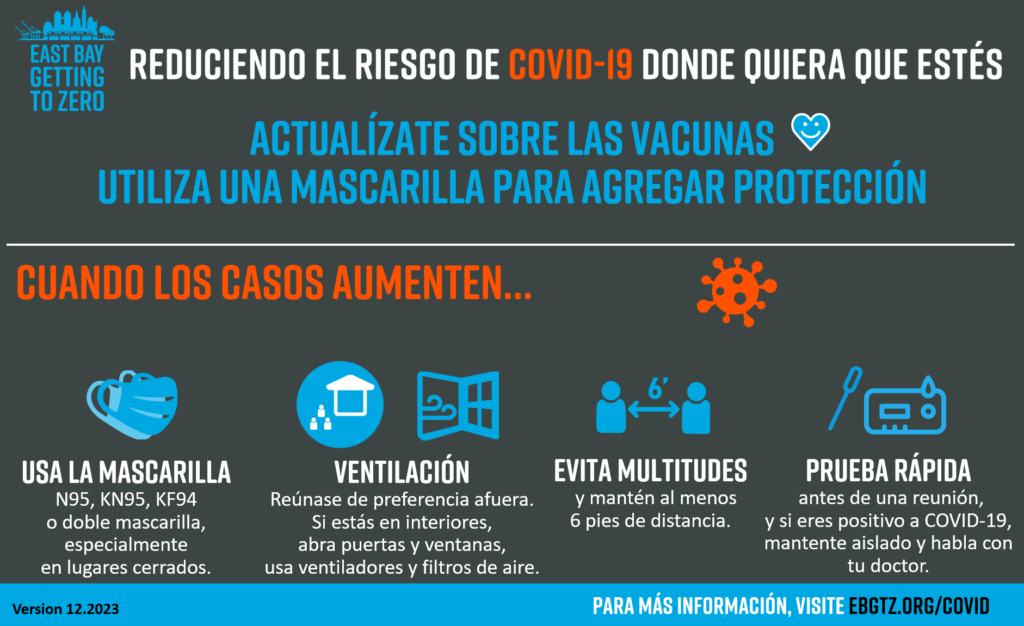
- Protect yourself and our communities by:
- staying home when you have symptoms,
- getting updated flu and Covid vaccines, and the RSV vaccine if you’re 60+
- wearing N95/KN95/KF94 masks,
- ventilating indoor spaces, and
- using rapid tests before gathering, when you have symptoms and after exposures.
- If you get Covid, talk to your provider about getting treatment or get a free virtual COVID visit here (1 (888) 897-1244). Roots has a helpful video on how to prevent the spread of COVID within your household.
Get an updated vaccine at local pharmacies, your medical provider, MyTurn.ca.gov, Vaccines.gov, or county sites.
Variants:
- Find the latest variant proportions: Bay Area & CA (click on COVID, variants, region) | US | US wastewater | Global
- Symptoms and severity appear to be similar across these Omicron subvariants.
- Rapid tests still work, thought not as well with the newer variants. Omicron variants tend to replicate in the throat earlier than the nose, so consider getting throat samples, then nose samples on the same swab.
- Boosters and antiviral treatment are still effective against severe disease from the newer variants.
- Read more about East Bay variants here.
Vaccines:
- Updated Covid vaccines are available in the East Bay and protect against the currently circulating variants. Get a booster to protect yourself and the community, especially if it’s been 6+ months since your last vaccine or infection.
- Adults ages 65 and older or are immunocompromised are now recommended by the CDC to receive an additional dose of the updated Covid vaccine as long as it’s been at least 2 months since their previous updated vaccine dose. For more info, please see CDC Covid vaccine guidance.
- The 2023-2024 updated Covid vaccines targeting XBB1.5 have been approved and recommended by the FDA and CDC for everyone ages 6 months and up.
- The updated vaccine protects against currently circulating variants in the East Bay: Updated vaccine data shows that it provides a significant increase in antibody response to the currently circulating variants, including EG.5, FL.1.5 and XBB1.16, as well as the highly mutated JN.1 variant. New data also shows that vaccinations reduce the risk of long Covid symptoms in adults and children.
- If you have insurance, check with your primary care clinic or pharmacy for the updated vaccine. They are most likely to provide the vaccine with the fewest insurance issues. Unlike before, insurance coverage will be checked before Covid vaccines are given at pharmacies. Coverage at specific pharmacies depends on their insurance contracts.
- If you don’t have insurance or your insurance doesn’t cover the complete Covid vaccine cost: CVS and Walgreens are required by the national Bridge Program to cover Covid vaccines at no cost to you. You can also go to designated public/county vaccine sites – click here for details.
- When to get the booster: you are eligible if your last vaccine dose was 2+ months ago. Generally, most people can wait 3 months after their last infection. To have protection for the anticipated winter wave, get it by early November.
- The Novavax COVID-19 vaccine is available at your local Walgreeens, CVS, and Costco pharmacies. The Novavax COVID-19 Vaccine, Adjuvanted, a monovalent vaccine, has been updated to include the Omicron variant lineage XBB.1.5 (2023-2024 formula). Please see this FDA Fact Sheet for more information. To schedule a vaccination appointment, please visit the website of your pharmacy of choice. Kaiser locations will offer the Novavax only to persons who were previously unable to receive the Pfizer or Moderna vaccines.
The CDC has updated their vaccine guidelines:
- Everyone ages 6 months and over should get at least one updated vaccine dose (Pfizer, Moderna or Novavax) to be considered up to date.
- People ages 65+ may get a 2nd updated booster dose at least 4 months after the first one.
- People who are moderately or severely immunocompromised may get additional updated doses at least 2 months after the previous one.
- Get an updated vaccine at local pharmacies, your medical provider, MyTurn.ca.gov, Vaccines.gov, or county sites.
Prevention:
- The CDC updated unified guidance for respiratory viruses in March 2024, including guidance for Covid, flu and RSV.
- Most guidance around prevention (vaccines, hygiene, ventilation, masks) is not changed.
- Isolation guidance now is similar to California’s and includes staying at home when you’re sick, then using masks and tests for 5 days after your symptoms get better to help prevent transmission.
- Updated 2024 data on this winter season’s Covid, flu and RSV severity and vaccine efficacy is published on Background for CDC’s Updated Respiratory Virus Guidance.
- California isolation and quarantine guidelines were updated in August 2023:
- Ventilation: The CDC released new indoor building ventilation standards in May 2023. They recommend aiming for at least 5 air exchanges per hour and using MERV-13 or better filters to reduce transmission of respiratory infections.
- Masks: New mask requirement for workers in high risk health settings, November 1, 2023 through April 30, 2024: Staff and other workers in specified health facilities (General Acute Care Hospitals, Long Term Acute Care Hospitals, Psychiatric Hospitals, Skilled Nursing Facilities, Dialysis Centers, and Infusion Centers) in Alameda County and Contra Costa County are required to wear high-quality, well-fitting masks in patient care areas. Sonoma and San Mateo counties will have the same requirement. San Francisco already has a year-round masking requirement for health care workers. Other individual facilities may still choose to make masks required.
- Want to test how well your mask fits? If you can’t get a professional mask fit-test, aerosol scientist Linsey Marr says you can informally test your mask by cupping “your hands around the edges and hold it down while you’re breathing through it and see if there’s any difference when you do that and press it to your face versus when you don’t. If you notice a difference, that means it’s not well sealed to your face and you should try a different type of mask.”
Test-and-treat:
- Free Covid tests are still available:
- Free PCR tests are available at the Community Church in Oakland on Tuesdays, Wednesdays and Thursdays 10:00am to 3:00pm at 1527 34th St Oakland, CA 94608. Register here, visit the Community Church website or call 510 594-2207 for more information.
- Free Covid-19 tests are back on COVIDtests.gov. Each US household can request another round of 4 free rapid tests through USPS if you haven’t ordered since November 20, 2023.
- People with health insurance in California can still get 8 free rapid tests per member per month. Some insurance plans (such as Kaiser) will continue to cover in-network rapid test kits after November 11, 2023.
- Umoja Health Community Hub offers free rapid antigen tests at their North Oakland site at 750 Aileen Street, Oakland 94609, Monday-Tuesday-Wednesday, 10 am to 2 pm, 1-888-763-0007. They offer N95s and other masks, hand sanitizer, rapid antigen tests and printed resources at this location.
- Contra Costa residents can get 4 additional free at-home COVID test kits per household by filling out this online form or by calling 833-829-2626.
- For in-person tests, contact your primary care clinic or find a testing site in California here.
- If you have symptoms, mask up and do serial antigen testing or get a PCR or other molecular test. Recent data shows that viral loads don’t peak until around Day 4 of symptoms with the Omicron variants. This means that antigen tests miss some infections in the first few days of symptoms. We have accumulated more immunity and are now more likely to have symptoms early in an infection. Another study also suggests that antigen levels might be lower than RNA levels with Omicron infections. What you can do to increase test accuracy:
- Omicron viral levels rise in the throat before the nose, so consider swabbing the throat before swabbing the nose.
- Repeat antigen testing has also been shown to increase accuracy in picking up infections. Current guidance is to repeat antigen testing 48 hours after the first negative test before excluding Covid infection.
- PCR tests still pick up early Omicron infections.
- Home molecular test kits are also available (Lucira COVID, Lucira COVID+flu, or Metrix COVID test kits), which detect viral genetic material like PCR tests. These home molecular tests are more sensitive and accurate than antigen tests, but they are also more expensive ($25-50 per test).
- Are expired COVID home tests still useful? If you still get a clear “control” line, the test is likely to still be effective.
- COVID test-and-treat: Paxlovid is still free and widely available! Community members at risk can get treatment at the same location and on the same day that you test positive and regardless of insurance or immigration status. Please encourage anyone who tests positive to contact their provider or a free test-and-treat center ASAP, as they may be able to get treatment.
- Free COVID clinical consults for CA clinicians: California health care providers can now call (866) 268-4322 (COVID-CA) to receive free and confidential consultation on COVID-19 testing and treatment from the UCSF National Clinician Consultation Center.
- What are current COVID treatment options?
- Paxlovid, remdesivir and molnupiravir remain effective against the newer variants.
- Viral rebound is common for both treated and untreated people with COVID-19. There is no evidence of resistance to Paxlovid. Treatment still helps reduce viral load and severity. Just make sure to re-isolate.
- Paxlovid expiration dates have been extended to 24 months by the FDA. Check updated expiration dates here.
- How can we prevent long COVID? Aside from wearing masks and preventing infection, the latest data suggests that you can reduce the risk of long COVID if you get infected with:
- Vaccination with at least 2 doses was associated with a 43% reduction of long COVID in a large systematic review of 41 studies.
- Paxlovid treatment was found to reduce the risk of long COVID by 26% in a large VA study.
- Metformin (a safe and inexpensive medication usually used for diabetes) taken for 2 weeks during acute COVID infection was found to reduce healthcare utilization for severe COVID and the development of long COVID symptoms by 42% in a randomized control trial.
- Ensitrelvir (a protease inhibitor like Paxlovid) taken once a day for 5 days was compared to placebo in a randomized control trial in people at lower risk (mostly ages 12-69, vaccinated, no medical risk factors for severe disease), and was found to reduce long Covid symptoms by 26-45%, shorten symptoms by a day and reduce time to first negative test. This study was also presented at CROI 2023. Ensitrelvir is already approved for COVID treatment in Japan.
- A “healthy lifestyle” (BMI 18-25, never smoking, exercise, moderate alcohol intake, high quality diet, sleeping 7-9 hours per day) was found in the Nurses’ Health Study II cohort (all women, 97% white) to be associated with a lower risk of long COVID. Participants with 5-6 healthy lifestyle factors had 49% lower risk of long COVID.
The end of COVID emergencies:
Free Covid vaccines, testing and treatment will still be covered by insurance and available at pharmacies and community partners for uninsured people after the federal public health emergency ends on May 11 under CA law, the national PREP Act and new Bridge Access Program.
Under California law: “After November 11, 2023, enrollees can continue to access COVID-19 tests, vaccines and treatment with no prior authorization or cost sharing when they access these services through their health plan’s network. Health plan enrollees can be charged cost-sharing only if these services are provided out of network after November 11, 2023.”
- In April 2023, the Department of Health and Human Services (DHHS) announced that some of the PREP Act protections for Covid vaccines and treatment distributed by the US through pharmacies and community partners will continue, including pharmacist-administered free vaccines and treatments and the national Covid test-to-treat program. The CA Covid test-to-treat program through Sesame care is also still available.
- DHHS also announced that they will partner with pharmacies to provide Covid vaccines and treatments such as Paxlovid free-of-charge to people without insurance coverage in the Bridge Access Program to be launched this fall.
- People with insurance coverage in California will be protected from out-of-pocket charges for Covid testing, vaccines and treatment from any licensed provider until November 11, 2023. After that, California insurance companies will still be required to cover these costs in-network without out-of-pocket charges. Click for more info about the end of the public health emergency for California residents.
California’s COVID state of emergency ended on February 28, 2023. The end of the state emergency has led to the end of extra pandemic-era CalFresh benefits and the closure of some COVID testing and treatment sites. It may also impact hospitals’ ability to address staffing and space shortages as well as some COVID-related paid medical leave policies. Click for more info about the end of the public health emergency for California residents.
The end of the federal emergency on May 11, 2023 will result in:
- The end of continuous Medi-Cal coverage. Medi-Cal recipients will have to manually renew and prove eligibility again.
- The end of national requirements for insurance to cover COVID-related costs. A CA law (CA Senate Bill 1473) extends this requirement for 6 more months to November 11, 2023, so insurance coverage of home test kits and COVID-related health care costs in California will extend till then.
- The end of requirements for insurance to cover all telehealth services; coverage will vary by state.
Click to read more about: the end of the California state emergency and the end of the federal emergency.
Latest COVID resources
Click here for more East Bay COVID guidance and resources on how to protect ourselves and our communities.